Introduction
Overview of Avian Influenza (Bird Flu)
Avian Influenza, commonly known as bird flu, is an infectious disease caused by influenza viruses that primarily affect birds. While most strains of bird flu are not harmful to humans, some have the potential to cross species barriers and infect people. The primary strains of avian influenza include various subtypes classified based on their surface proteins, hemagglutinin (H) and neuraminidase (N). In 2024, the H5N1 strain has emerged as a major concern due to its potential for causing severe illness in both birds and mammals, including humans.
Introduction to the Concept of Bird Flu and Its Significance in 2024
Bird flu has been a known concern since its first identification in the 1950s, but the current 2024 context presents new challenges. The significance of bird flu in 2024 is underscored by its rapid spread among various species and its potential to cause a global health crisis. Unlike earlier outbreaks, the current strain has demonstrated an alarming ability to infect a wider range of animals, including dairy cattle and even some mammals, which raises the stakes for human health and pandemic preparedness.
The ongoing bird flu pandemic in 2024 is characterized by an unprecedented level of surveillance and concern from global health authorities. The virus has not only impacted avian populations but has also been detected in several mammalian species, including cattle, raising concerns about its adaptability and potential to cause a new pandemic.”
Dinfected humans, often with severe consequences.
In recent years, H5N1 has evolved, showing an increased capacity to infect different species beyond birds, including mammals like cattle and even dolphins. This broader host range has heightened concerns about the virus’s potential to become more adaptable and transmissible. The 2024 outbreak has seen significant numbers of infections in both domestic and wild birds, as well as infections in dairy cattle across multiple states, further complicating the public health response.
The persistence and evolution of the H5N1 strain underscore the importance of ongoing surveillance and research to understand its behavior and to prepare for potential scenarios where it could pose a serious threat to human health. Efforts are currently focused on monitoring the virus’s genetic changes, evaluating its impact on various species, and developing strategies to prevent and control its spread.
2. Bird Flu Pandemic 2024

Bird Flu: The Emerging Pandemic Threat and How Medicine is Fighting Back
Explore the growing threat of bird flu as it emerges as a potential pandemic. Delve into the latest pharmacological interventions, vaccine developments, and global health strategies to combat this evolving virus. Learn about the impact on public health and preventive measures being taken. For a comprehensive overview, refer to the detailed PDF document linked here.
Emergence and Spread of Bird Flu
Timeline of Bird Flu’s Detection and Spread from 2020 to 2024

Image Reference:- A geospatial perspective towards the role of migratory birds and poultry in the spread of Avian Influenza – Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Timeline-of-H5N1-Strain-Development-1900-2024_fig1_381172951 [accessed 1 Sept 2024]
The bird flu pandemic has evolved significantly from its early detections to the current state in 2024. Here’s a detailed timeline of key events:
- 2020: The H5N1 avian influenza strain began to make headlines as it was detected in several countries, including the United States. Early cases were primarily confined to wild birds and poultry, with limited transmission to other species.
- 2021-2022: The virus continued to spread among wild birds and poultry populations. Several outbreaks were reported globally, leading to large-scale culling of infected birds to prevent further spread. Surveillance and research efforts increased to monitor the virus’s evolution and its potential impact on other species.
- 2023: The H5N1 strain showed signs of adaptation, with reported infections in mammals, including several species of wild animals. This period marked a significant shift as the virus began to affect animals beyond birds, raising alarms among health authorities.
- 2024: The virus’s spread has intensified, with notable recent cases, including a significant infection in dairy cattle in Texas. The virus has been detected in over 34 herds across nine states. Infections in mammals, including cattle and dolphins, have further complicated containment efforts.
Detailed Account of Recent Cases, Including the Infection in Texas and Its Implications


The latest developments in the bird flu pandemic are marked by a notable case in Texas, where a dairy worker contracted the H5N1 virus. This case represents a critical juncture in the pandemic, as it indicates the virus’s potential to cross species barriers and infect humans.
- Texas Infection: In early 2024, health officials reported that a dairy worker in Texas tested positive for H5N1. This infection is particularly concerning because it highlights the virus’s ability to infect mammals and potentially transmit to humans. The case led to increased scrutiny and testing in agricultural environments to prevent further spread.
- Implications: The detection of H5N1 in Texas and other regions underscores the growing risk of the virus evolving to become more transmissible among humans. It also stresses the need for robust surveillance and preventive measures in both animal and human populations.
Discussion of How the Virus Spread Rapidly Among Wild Birds, Poultry, and Mammals
The rapid spread of the H5N1 virus can be attributed to several factors:
- Wild Birds: Migratory patterns have facilitated the spread of the virus across continents. Wild birds often carry the virus over long distances, contributing to widespread outbreaks in poultry farms and other avian populations.

- Poultry: The virus has had a devastating impact on the poultry industry, with millions of birds culled to prevent outbreaks. The dense population of birds in commercial poultry operations has provided an ideal environment for the virus to spread rapidly.

- Mammals: Recent findings of H5N1 in mammals, including cattle and dolphins, suggest that the virus is adapting to new hosts. This adaptation poses a significant challenge for containment efforts and increases the risk of the virus potentially evolving to infect humans more efficiently.

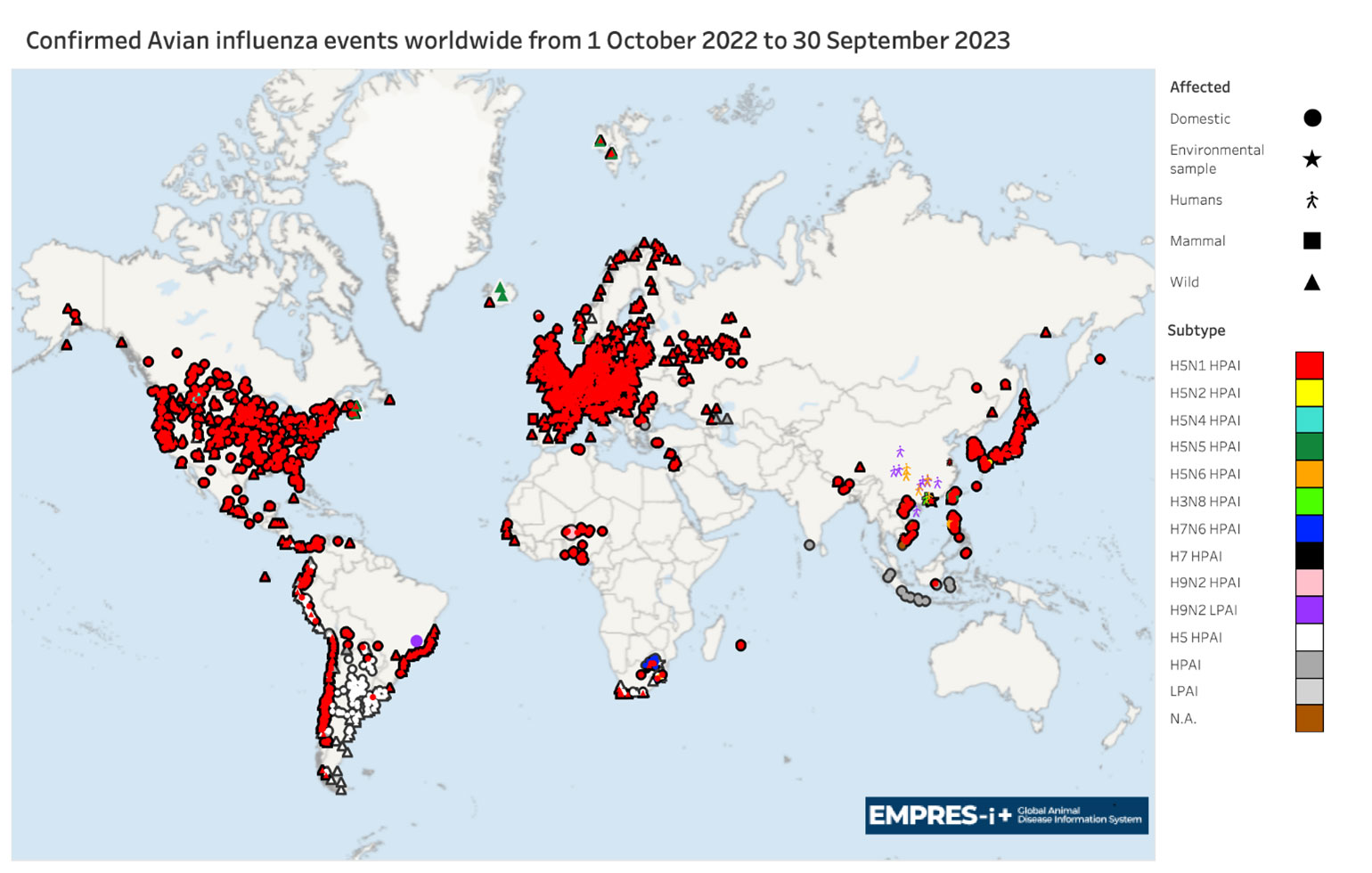
Current Avian Flu Map
Visual Representation of Bird Flu’s Spread Across Different Regions
A detailed map of avian flu’s current spread provides a clear visualization of the virus’s impact globally. The map highlights the following:
- Global Hotspots: Major outbreaks are marked in regions such as North America, Europe, and parts of Asia. These areas have reported significant numbers of cases in both avian and mammalian populations.
- United States: Within the U.S., hotspots include several states where the virus has been detected in poultry and dairy cattle. The states with the highest concentrations of cases are highlighted to show the regions most affected.
Highlight Affected Areas Globally, Including Hotspots in the United States
- North America: The U.S. and Canada have reported numerous cases, with recent outbreaks in Texas and other states raising concerns. The map shows areas with ongoing surveillance and containment efforts.
- Europe and Asia: Countries such as the United Kingdom, France, and several Asian nations are also affected. The map highlights these regions as they experience ongoing challenges with bird flu outbreaks.
Impact on Agriculture and Public Health
How the Bird Flu Pandemic Has Affected the Poultry Industry
- Poultry Industry: The bird flu pandemic has caused significant disruptions in the poultry industry. Millions of birds have been culled to control outbreaks, leading to substantial economic losses and disruptions in the supply chain. The poultry industry faces challenges in recovering from these losses and managing the ongoing threat of the virus.
Impact on Dairy Cattle and the Detection of the Virus in Milk Supplies
- Dairy Cattle: The recent detection of H5N1 in dairy cattle represents a new concern for the agriculture sector. Infected cattle have led to heightened scrutiny of dairy products, though pasteurization processes effectively kill the virus.
- Milk Supplies: Despite the detection of the virus in milk, health authorities assure that commercially bought milk remains safe due to pasteurization. However, the detection has prompted increased testing and monitoring to ensure food safety.
Economic Implications and Public Health Concerns
- Economic Implications: The economic impact of the bird flu pandemic includes losses in the poultry industry, increased costs for monitoring and containment, and potential disruptions in agricultural markets. The broader economic consequences may affect related industries and supply chains.
- Public Health Concerns: The potential for H5N1 to evolve and infect humans raises significant public health concerns. Authorities are focusing on preparedness and response strategies to mitigate the risk of a more severe outbreak and protect public health.
How Does Bird Flu Spread to Humans?

Transmission Mechanisms
Detailed Explanation of How Bird Flu Viruses Are Transmitted from Birds to Humans
Bird flu, particularly the H5N1 strain, is primarily an avian disease, but it can occasionally jump to humans through various transmission mechanisms. Understanding these pathways is crucial to preventing and controlling potential outbreaks.
- Direct Contact with Infected Birds: The most common way bird flu spreads to humans is through direct contact with infected birds. This includes handling birds, feathers, or bird droppings. Farmers, poultry workers, and those involved in the culling of infected birds are at the highest risk. The virus can enter the human body through mucous membranes in the eyes, nose, or mouth, or through cuts and abrasions on the skin.
- Consumption of Contaminated Products: Another potential transmission route is through the consumption of raw or undercooked poultry products, such as meat or eggs. Although cooking at high temperatures kills the virus, handling contaminated products during preparation can pose a risk, especially if proper hygiene practices are not followed.
- Environmental Exposure: Bird flu can also spread through environmental exposure. The virus can survive in bird droppings, contaminated water, and on surfaces for extended periods. In agricultural settings, workers may inhale dust or aerosols that contain the virus, leading to infection.
Analysis of Specific Cases Where Human Infection Occurred, Such as Farm Workers and Dairy Cattle Handlers
Recent cases of human infection provide insight into how bird flu can spread from animals to humans:
- Farm Workers: Many documented cases of H5N1 infection have occurred in farm workers who are in close contact with poultry. In these instances, the virus was transmitted through direct handling of infected birds or exposure to contaminated environments. For example, in Asia, where several outbreaks occurred, farm workers who were not wearing protective gear were particularly vulnerable.
- Dairy Cattle Handlers: The recent detection of H5N1 in dairy cattle in Texas highlights a new risk group—dairy workers. In one notable case, a dairy worker contracted the virus, likely through close contact with infected cattle or contaminated milk. Although the virus found in milk was not live due to pasteurization, the worker’s infection suggests that other factors, such as environmental exposure or handling of infected animals, played a role.
Role of Direct Contact with Infected Birds, Consumption of Contaminated Products, and Environmental Exposure
Each transmission pathway presents unique risks:
- Direct Contact: Direct contact remains the most significant risk for humans. The virus can transfer easily through handling infected birds or their secretions. The absence of protective equipment and the presence of open wounds increase the likelihood of transmission.
- Contaminated Products: While the consumption of contaminated products, especially raw or undercooked poultry, is less common as a transmission route, it is still a concern. The virus does not survive well at high temperatures, so cooking effectively reduces this risk. However, cross-contamination during food preparation remains a potential hazard.
- Environmental Exposure: In farming environments, the virus can persist in bird droppings, water, and other materials. Aerosolized particles from bird droppings can infect individuals who inhale them, particularly in confined spaces with poor ventilation. This environmental exposure poses a risk not only to farm workers but also to those living in close proximity to infected farms.
Human-to-Human Transmission Potential
Examination of the Possibility of the Virus Mutating to Allow Human-to-Human Transmission
The possibility of H5N1 mutating to allow efficient human-to-human transmission is a significant concern among scientists and public health officials. While current strains of bird flu are not easily transmissible between humans, there is always a risk that the virus could mutate or reassort with human influenza viruses, potentially creating a strain capable of widespread human transmission.
- Mutation and Reassortment: Influenza viruses, including H5N1, have the ability to mutate rapidly. These mutations can occur randomly or through reassortment, where genetic material from different influenza strains combines. If H5N1 were to acquire mutations that allow it to bind more effectively to human respiratory cells, it could lead to sustained human-to-human transmission.
- Current Cases and Implications: While most human cases of H5N1 have resulted from direct contact with infected birds, there have been isolated instances where limited human-to-human transmission may have occurred. These cases typically involve close contact between individuals, such as family members or healthcare workers. Although these instances did not result in widespread transmission, they underscore the potential for the virus to evolve.
Insights from Experts Like Dr. Robert Redfield on the Potential Risks
Experts in the field, such as former CDC Director Dr. Robert Redfield, have expressed concerns about the potential for H5N1 to become a pandemic threat. According to Dr. Redfield, the virus’s ability to spread across species, including mammals, is alarming. He emphasizes the need for vigilance and preparation to mitigate the risk of a future pandemic.
- Dr. Redfield’s Perspective: Dr. Redfield has highlighted the importance of monitoring the virus’s genetic changes and understanding how these changes could impact transmission. He warns that the world must take the threat seriously, especially given the virus’s high mortality rate in humans.
Discussion on the “Species Barrier” and How the Virus Could Overcome It
The “species barrier” refers to the natural resistance that typically prevents viruses from easily jumping from one species to another. For H5N1, this barrier has largely kept the virus confined to birds, with only rare instances of human infection. However, this barrier is not impenetrable, and certain factors could allow the virus to overcome it:
- Viral Adaptation: As H5N1 continues to infect a broader range of animals, including mammals, the virus is given more opportunities to adapt to new hosts. Each infection in a new species presents a chance for the virus to acquire mutations that could help it infect humans more effectively.
- Environmental Pressures: High-density farming, climate change, and increased human-animal interactions are all factors that could pressure the virus to adapt. For instance, in densely populated farms, the virus has more opportunities to mutate and find pathways to overcome the species barrier.
- Surveillance and Containment: Continuous surveillance of the virus in animal populations is crucial to detect these mutations early. Containment measures, such as culling infected animals and restricting movement in outbreak areas, are essential to preventing the virus from overcoming the species barrier.
In conclusion, while bird flu remains predominantly an avian disease, the possibility of it spreading to humans through various transmission mechanisms is real. The potential for the virus to mutate and allow human-to-human transmission is a significant concern that requires ongoing vigilance and preparedness.
Symptoms of Bird Flu in Humans

Early Signs and Symptoms
Detailed Overview of the Symptoms of Bird Flu in Humans
Bird flu, particularly the H5N1 strain, presents a range of symptoms in humans that can vary in severity. Understanding these symptoms is essential for early detection and treatment, which can be life-saving.
- Fever and Cough: The initial symptoms of bird flu are often similar to those of the seasonal flu. Patients typically experience a high fever, often exceeding 100.4°F (38°C), accompanied by a persistent cough. These early signs can easily be mistaken for a common respiratory infection.
- Sore Throat and Muscle Aches: Along with fever and cough, many patients report a sore throat and muscle aches (myalgia). These symptoms contribute to the general malaise and fatigue that characterize the early stages of the illness.
- Headaches and Runny Nose: Headaches are another common symptom, often described as severe and persistent. Some patients may also experience a runny or stuffy nose, though this is less common than other flu-like symptoms.
- Conjunctivitis (Eye Infection): In some cases, bird flu can cause conjunctivitis, leading to redness, swelling, and discharge from the eyes. This symptom is more specific to bird flu and is a key differentiator from seasonal flu.
Differentiating Between Mild and Severe Symptoms, Including Respiratory Distress and Pneumonia
As the disease progresses, symptoms can worsen, leading to severe respiratory issues:
- Shortness of Breath: A hallmark of severe bird flu infection is difficulty breathing or shortness of breath, which usually develops a few days after the onset of initial symptoms. This symptom indicates that the virus is affecting the lungs, leading to more serious complications.
- Pneumonia: Pneumonia is one of the most serious complications of bird flu, often developing quickly after the initial respiratory symptoms. It occurs when the virus causes inflammation and fluid buildup in the lungs, leading to severe respiratory distress. Patients with pneumonia require immediate medical attention, as it can be life-threatening.
- Respiratory Failure: In severe cases, bird flu can lead to acute respiratory distress syndrome (ARDS), a condition where the lungs cannot provide enough oxygen to the body’s vital organs. This can result in respiratory failure, requiring mechanical ventilation and intensive care.
- Gastrointestinal Symptoms: Some patients with bird flu may also experience gastrointestinal symptoms such as diarrhea, abdominal pain, and vomiting. These symptoms are less common but can occur, particularly in severe cases.
H5N1 Symptoms
Specific Focus on Symptoms Associated with the H5N1 Strain
The H5N1 strain of bird flu is known for its severity and high mortality rate. The symptoms associated with H5N1 are often more severe than those of other strains:
- High Fever and Severe Cough: Patients infected with H5N1 often experience a very high fever, typically above 102°F (39°C). The cough associated with H5N1 is usually dry and severe, leading to significant discomfort and difficulty breathing.
- Chest Pain and Difficulty Breathing: Chest pain is a common symptom in H5N1 cases, often linked to the development of pneumonia. The difficulty in breathing can escalate quickly, necessitating urgent medical intervention.
- Bleeding from the Nose and Gums: In some H5N1 cases, patients may experience bleeding from the nose or gums, a symptom not commonly seen in seasonal flu. This bleeding is a sign of severe infection and can indicate a poor prognosis.
- Altered Mental Status: Severe cases of H5N1 may also involve neurological symptoms, such as confusion, seizures, or altered mental status. These symptoms suggest that the virus is affecting the central nervous system, leading to more serious complications.
Comparison with Symptoms of Seasonal Flu and Other Viral Infections
It is important to differentiate H5N1 symptoms from those of seasonal flu and other viral infections:
- Severity of Symptoms: While seasonal flu can cause significant discomfort, H5N1 symptoms are typically more severe and escalate more quickly. The progression from mild symptoms to severe respiratory distress is much faster in H5N1 infections.
- Mortality Rate: The mortality rate for H5N1 is significantly higher than that of seasonal flu. While seasonal flu has a mortality rate of less than 0.1%, H5N1 can have a mortality rate as high as 52%, making it one of the deadliest strains of influenza.
- Gastrointestinal and Neurological Symptoms: While seasonal flu rarely causes gastrointestinal or neurological symptoms, these are more common in H5N1 cases, further distinguishing it from less severe flu strains.
Severity and Mortality Rates

Analysis of the Mortality Rate of Bird Flu Compared to Other Flu Strains, Including COVID-19
Bird flu, particularly the H5N1 strain, is associated with a much higher mortality rate compared to other flu strains:
- H5N1 Mortality Rate: The World Health Organization (WHO) reports that approximately 52% of individuals infected with H5N1 have died since its first detection in humans in 1997. This makes H5N1 one of the most lethal strains of influenza.
- Comparison with Seasonal Flu: In contrast, seasonal flu has a much lower mortality rate, typically around 0.1%. This vast difference underscores the deadly potential of H5N1 if it were to become more transmissible among humans.
- Comparison with COVID-19: At the start of the COVID-19 pandemic, the fatality rate was estimated to be around 1-2%, although this has varied based on region, age, and access to healthcare. Even at its peak, COVID-19’s mortality rate was far lower than that of H5N1, highlighting the potential danger of an H5N1 pandemic.
Case Studies Highlighting the Fatality Rates of H5N1, with a Focus on the 52% Mortality Rate
Several case studies demonstrate the high fatality rate of H5N1:
- Indonesia 2005-2006: During an outbreak of H5N1 in Indonesia, 45 out of 61 confirmed cases resulted in death, reflecting a mortality rate of 74%. Many of these cases involved direct contact with infected poultry, and the rapid progression of the disease was a common factor in fatalities.
- Egypt 2009: In Egypt, H5N1 outbreaks resulted in a 34% mortality rate, with 264 confirmed cases and 89 deaths. The majority of those affected were involved in poultry farming, and delays in seeking medical treatment contributed to the high fatality rate.
- Vietnam 2004-2005: Vietnam experienced a significant outbreak of H5N1, with a mortality rate of 50%. Out of 112 confirmed cases, 56 individuals died. The outbreak highlighted the challenges of managing bird flu in regions with high poultry density and limited healthcare resources.
Can Bird Flu Kill Humans?
Exploration of the Lethality of Bird Flu in Humans
The lethality of bird flu, particularly the H5N1 strain, is well-documented. The virus’s ability to cause severe respiratory illness, coupled with its high mortality rate, makes it a significant public health threat.
- High Mortality Rate: As mentioned, H5N1 has a mortality rate of about 52%, making it one of the deadliest viruses known to infect humans. The high fatality rate is largely due to the virus’s ability to cause severe lung damage and respiratory failure.
- Potential for Mutation: The potential for the virus to mutate and become more easily transmissible among humans increases the risk of a widespread and lethal pandemic. Public health experts are particularly concerned about the virus’s capacity to evolve, which could lead to a scenario where bird flu becomes as contagious as seasonal flu but far more deadly.
Historical Data on Bird Flu Fatalities Globally Since 2003

Since the first human cases of H5N1 were detected in 1997, there have been numerous outbreaks across the globe, leading to hundreds of fatalities:
- Global Fatalities: According to the WHO, there have been over 860 confirmed cases of H5N1 globally, with more than 450 deaths since 2003. These numbers reflect the high lethality of the virus, particularly in regions with close human-animal interactions.
- Asia as a Hotspot: The majority of bird flu fatalities have occurred in Asia, particularly in countries like Indonesia, Vietnam, and China, where poultry farming is widespread, and human-bird contact is common. These regions have seen the highest number of cases and deaths, highlighting the need for stringent biosecurity measures.
- Ongoing Threat: Despite advancements in detection and prevention, bird flu remains a persistent threat, with new cases emerging sporadically. The continued presence of the virus in wild and domestic bird populations poses an ongoing risk of human infection and potential fatalities.
In summary, the symptoms of bird flu in humans range from mild flu-like signs to severe respiratory distress and death. The H5N1 strain, in particular, is associated with a high mortality rate, making it one of the most dangerous influenza viruses. Understanding the symptoms, transmission mechanisms, and potential lethality of bird flu is crucial for early detection, treatment, and prevention of future outbreaks.
H5N1: The Strain of Concern

Genetic Composition and Evolution
Overview of the H5N1 Strain’s Genetic Makeup and How It Differs from Other Flu Strains
H5N1, also known as avian influenza A, is a subtype of the influenza virus that primarily infects birds but has also been known to infect humans and other animals. The “H” in H5N1 stands for hemagglutinin, and the “N” stands for neuraminidase, which are two types of proteins found on the surface of the virus. Hemagglutinin (H) allows the virus to bind to and enter host cells, while neuraminidase (N) enables the release of new viral particles from infected cells, allowing the infection to spread.
The H5N1 strain is particularly concerning due to its unique genetic composition:

- High Pathogenicity: H5N1 is classified as a highly pathogenic avian influenza (HPAI) virus, meaning it can cause severe disease and death in birds. This high pathogenicity is linked to specific mutations in the hemagglutinin gene, which increases the virus’s ability to infect cells and evade the host’s immune response.
- Differences from Seasonal Flu: Unlike seasonal flu strains, which have a lower mortality rate and typically cause mild to moderate illness in humans, H5N1 has a significantly higher mortality rate. This is partly due to its ability to cause a hyper-inflammatory response in the body, leading to severe respiratory distress and multi-organ failure.
- Genetic Reassortment: H5N1 has a segmented genome, meaning its genetic material is divided into separate pieces of RNA. This allows for genetic reassortment, where different strains of the virus can exchange genetic material. This process can lead to the emergence of new, potentially more dangerous strains, particularly if H5N1 were to combine with a human influenza virus.
Discussion on the Virus’s Ability to Mutate and Adapt, Increasing Its Threat to Humans
The H5N1 virus has shown a remarkable ability to mutate and adapt, which increases its potential threat to humans:
- Mutation Rate: Influenza viruses, including H5N1, have a high mutation rate due to the lack of proofreading mechanisms during viral replication. This leads to frequent changes in the virus’s genetic makeup, allowing it to adapt to new hosts, including humans.
- Adaptation to Mammals: While H5N1 primarily infects birds, mutations in the virus have enabled it to infect mammals, including humans. These adaptations include changes in the virus’s hemagglutinin protein, allowing it to bind more effectively to mammalian cells.
- Potential for Human-to-Human Transmission: Although human-to-human transmission of H5N1 is currently rare, the virus’s ability to mutate raises concerns that it could acquire this capability. If H5N1 were to mutate in a way that allows efficient transmission between humans, it could lead to a global pandemic with a high mortality rate.
The Role of “Gain-of-Function” Research and Its Ethical Implications
“Gain-of-function” (GOF) research involves altering the genetic makeup of viruses to study their potential to cause disease. This type of research has been conducted on H5N1 to understand how it might mutate to become more transmissible among humans. While GOF research has provided valuable insights, it is also highly controversial due to the associated risks:
- Purpose of GOF Research: The primary goal of GOF research on H5N1 is to anticipate how the virus might evolve and to develop strategies for preventing or mitigating a potential pandemic. By understanding the genetic changes that could make H5N1 more transmissible or virulent, scientists aim to improve surveillance, develop vaccines, and design antiviral drugs.
- Ethical Concerns: Critics of GOF research argue that the risks may outweigh the benefits. Manipulating viruses to make them more dangerous poses the risk of accidental release from laboratories, which could potentially trigger a pandemic. Additionally, there are concerns about the dual-use nature of GOF research, as the same knowledge could be used to create bioweapons.
- Global Debate: The ethical debate surrounding GOF research has led to international discussions about the regulation and oversight of such experiments. Some countries have imposed moratoriums on GOF research, while others continue to support it under strict safety protocols. The World Health Organization (WHO) and other global bodies have called for a balanced approach that weighs the scientific benefits against the potential risks.
Global Impact and Response
Summary of the Global Response to H5N1, Including Surveillance, Testing, and Vaccine Development
The global response to H5N1 has involved a coordinated effort to monitor, detect, and prevent the spread of the virus. Key components of this response include:
- Surveillance: Surveillance programs have been established worldwide to monitor the spread of H5N1 in bird populations and to detect any spillover into humans. These programs involve routine testing of wild and domestic birds, as well as monitoring human cases, particularly in regions where the virus is endemic.
- Testing: Rapid diagnostic tests have been developed to detect H5N1 infections in both animals and humans. These tests are crucial for early detection and containment of outbreaks. In addition, molecular techniques such as polymerase chain reaction (PCR) are used to identify specific strains of the virus and track its genetic evolution.
- Vaccine Development: Developing a vaccine for H5N1 has been a priority for public health agencies. Several candidate vaccines have been developed and stockpiled in case of a pandemic. However, creating an effective and widely available vaccine is challenging due to the virus’s ability to mutate. Ongoing research is focused on developing universal flu vaccines that can protect against multiple strains, including H5N1.
WHO’s Role in Monitoring the Spread of H5N1 and Advising Countries on Preparedness
The World Health Organization (WHO) plays a central role in the global response to H5N1:
- Monitoring and Reporting: WHO coordinates global surveillance efforts and maintains a database of confirmed H5N1 cases in humans and animals. The organization also issues regular updates on the virus’s spread and advises countries on potential risks.
- Guidance on Preparedness: WHO provides guidelines and recommendations to countries on how to prepare for and respond to H5N1 outbreaks. This includes advice on surveillance, laboratory testing, infection control measures, and the use of antiviral drugs and vaccines.
- International Collaboration: WHO facilitates collaboration between countries, sharing data, research findings, and best practices. The organization also works with other international bodies, such as the Food and Agriculture Organization (FAO) and the World Organisation for Animal Health (OIE), to address the animal and human health aspects of H5N1.
Bird Flu Symptoms in Mammals and Birds
Symptoms Observed in Birds, Cattle, and Other Mammals
Bird flu, particularly the H5N1 strain, manifests differently in birds, cattle, and other mammals:
- Birds: In birds, H5N1 can cause a range of symptoms depending on the species and the virus’s pathogenicity. Highly pathogenic avian influenza (HPAI) viruses like H5N1 can cause sudden death in birds without any preceding signs. Infected birds may also show symptoms such as respiratory distress, coughing, sneezing, swollen wattles and combs, diarrhea, and a drop in egg production. Wild birds often serve as asymptomatic carriers, spreading the virus without showing severe illness.
- Cattle: The detection of H5N1 in cattle is relatively rare, but when it occurs, the symptoms can include respiratory distress, fever, and decreased milk production. Infected cattle may also exhibit signs of general malaise, such as lethargy and loss of appetite. The presence of the virus in cattle is concerning as it indicates a broader host range for H5N1, increasing the risk of transmission to humans.
- Other Mammals: H5N1 has been detected in various mammals, including domestic pets (such as cats and dogs), as well as wild mammals like tigers, leopards, and dolphins. Symptoms in mammals can include respiratory distress, fever, neurological signs such as seizures or ataxia, and, in severe cases, death. The infection of mammals with H5N1 is significant as it suggests the virus’s potential to jump species barriers and adapt to new hosts.
How the Symptoms in Animals Differ from Those in Humans
While H5N1 causes severe respiratory symptoms in both animals and humans, there are some key differences:
- Severity: In animals, particularly birds, H5N1 often causes more rapid and severe symptoms, leading to high mortality rates. In humans, the disease may progress more slowly, allowing for medical intervention, although the mortality rate remains high.
- Respiratory vs. Systemic Symptoms: In birds, H5N1 primarily causes respiratory symptoms, but it can also lead to systemic infection, affecting multiple organs. In humans, the virus typically starts with respiratory symptoms but can progress to systemic involvement, including severe pneumonia, multi-organ failure, and neurological symptoms.
- Transmission Dynamics: In animals, H5N1 spreads primarily through direct contact with infected individuals or contaminated environments. In humans, while direct contact with infected birds or contaminated surfaces is the main transmission route, the possibility of human-to-human transmission remains a concern, particularly if the virus mutates.
In conclusion, H5N1 remains a strain of significant concern due to its high pathogenicity, ability to mutate, and potential to cause severe disease in both animals and humans. Understanding its genetic composition, the global response to its spread, and the symptoms
Current Avian Flu Map and Spread
Geographical Spread and Affected Regions

Note: Symbols may overlap for events in similar geographic locations.
Note: Symbols may overlap for events in similar geographic locations.
Detailed Discussion of the Spread of Bird Flu Globally
The bird flu, particularly the H5N1 strain, has seen significant spread across various regions globally, with its impact being felt in numerous countries. The virus, which initially emerged in Southeast Asia in the late 1990s, has since spread to other parts of Asia, Europe, Africa, and North America, demonstrating its ability to cross borders and affect diverse ecosystems.
- Asia: Asia has been the epicenter of the H5N1 virus since its emergence. Countries like China, Vietnam, Indonesia, and Thailand have experienced recurrent outbreaks, with the virus becoming endemic in some regions. The spread in Asia is particularly concerning due to the region’s large poultry industry and the practice of live bird markets, which create ideal conditions for the virus to spread. Additionally, the close proximity of humans and animals in rural areas increases the risk of zoonotic transmission.
- Europe: The virus spread to Europe in the mid-2000s, with significant outbreaks reported in countries such as Germany, France, and the United Kingdom. Migratory birds played a key role in the transmission of the virus to Europe, bringing the disease from affected regions in Asia. In recent years, Europe has seen sporadic outbreaks, particularly during the winter months when migratory birds return from their breeding grounds in Asia.
- Africa: The spread of H5N1 to Africa was first documented in 2006, with Egypt being one of the hardest-hit countries. The virus spread rapidly across the continent, affecting both wild and domestic birds. The spread in Africa has been exacerbated by limited resources for disease surveillance and control, leading to ongoing challenges in managing the virus.
- North America: North America experienced its first major H5N1 outbreak in 2014-2015, affecting poultry farms across the United States and Canada. The virus was likely introduced by migratory birds from Asia, highlighting the interconnectedness of global ecosystems. The outbreak led to the culling of millions of birds, with significant economic losses for the poultry industry. More recently, in 2024, cases have been reported in Texas, raising concerns about the virus’s resurgence in the region.
- Other Regions: H5N1 has also been detected in other parts of the world, including the Middle East and South America. While the outbreaks in these regions have been less frequent, they underscore the virus’s ability to spread across continents and affect a wide range of species.
Current Status in Different Regions, Including North America, Europe, and Asia
As of 2024, the status of H5N1 varies across different regions:
- North America: The United States has seen a resurgence of H5N1 cases, particularly in Texas, where the virus was detected in dairy cattle. This has raised concerns about the virus spreading to other states and potentially affecting the broader agricultural industry. Surveillance efforts have been ramped up to monitor the spread of the virus and to prevent further outbreaks.
- Europe: Europe continues to experience sporadic outbreaks of H5N1, particularly in countries with large poultry industries. The virus has been detected in both wild and domestic birds, with culling measures implemented to contain the spread. The European Union has issued guidelines for member states to enhance biosecurity measures and to monitor migratory bird populations, which are a key vector for the virus.
- Asia: In Asia, H5N1 remains endemic in several countries, with regular outbreaks reported in both birds and humans. The region’s large population, coupled with the close interaction between humans and animals, makes it a hotspot for the virus. Governments in the region have implemented various measures to control the spread, including vaccination campaigns, culling of infected birds, and public health campaigns to raise awareness of the risks associated with bird flu.
- Africa: In Africa, the virus continues to pose a threat, particularly in countries with limited resources for disease control. Egypt remains one of the most affected countries, with regular outbreaks reported in both birds and humans. The virus’s persistence in the region highlights the need for sustained efforts to control its spread and to prevent zoonotic transmission.
- Other Regions: In the Middle East and South America, the virus is monitored closely, although outbreaks have been less frequent. The focus in these regions is on preventing the introduction of the virus through strict import controls and surveillance of wild bird populations.
Impact on Wildlife and Ecosystems
Effects of the Virus on Wild Bird Populations and Other Wildlife
The impact of H5N1 on wildlife, particularly wild bird populations, has been profound. The virus has led to mass die-offs of birds in various regions, disrupting local ecosystems and threatening biodiversity.
- Wild Bird Populations: Wild birds, particularly migratory species, have been significantly affected by H5N1. The virus has caused large-scale mortality events, particularly among waterfowl such as ducks, geese, and swans. These birds often serve as reservoirs for the virus, spreading it across continents during their migratory journeys. The loss of these species can have cascading effects on ecosystems, as they play key roles in seed dispersal, pest control, and nutrient cycling.
- Threatened and Endangered Species: H5N1 poses a particular threat to endangered bird species, which may already be struggling due to habitat loss and other factors. For example, the virus has been detected in populations of rare species such as the Oriental white stork and the red-crowned crane, raising concerns about their long-term survival.
- Other Wildlife: The spread of H5N1 to mammals, including species such as tigers and leopards, has highlighted the virus’s ability to jump species barriers. Infected mammals often suffer severe symptoms, including respiratory distress and neurological issues, leading to high mortality rates. The impact on these species is of particular concern in regions where they are already threatened by habitat loss and poaching.
Discussion on the Ecological Impact and Potential Long-Term Consequences
The ecological impact of H5N1 extends beyond the immediate effects on individual species, with potential long-term consequences for ecosystems:
- Disruption of Food Chains: The mass die-off of birds can disrupt food chains, particularly in ecosystems where birds play a crucial role as predators or prey. For example, the loss of waterfowl can affect populations of fish and invertebrates that rely on them for food, leading to imbalances in aquatic ecosystems.
- Ecosystem Services: Birds provide essential ecosystem services, such as pollination, seed dispersal, and pest control. The loss of bird populations due to H5N1 could reduce the availability of these services, affecting agricultural productivity and forest regeneration.
- Biodiversity Loss: The spread of H5N1 could contribute to the loss of biodiversity, particularly if the virus continues to affect endangered species. The decline or extinction of these species would reduce the genetic diversity of ecosystems, making them more vulnerable to other environmental stressors.
- Long-Term Consequences: The long-term consequences of H5N1 on ecosystems are still not fully understood, but the potential for ongoing disruptions is clear. If the virus continues to spread and mutate, it could lead to further losses of wildlife and changes in ecosystem dynamics. Conservation efforts will need to be enhanced to protect vulnerable species and to mitigate the ecological impact of the virus.
In summary, the current avian flu map and the spread of H5N1 highlight the virus’s global reach and its significant impact on wildlife and ecosystems. The ongoing spread of the virus poses a serious threat to biodiversity, with potential long-term consequences for ecosystems worldwide. Efforts to monitor and control the virus will be critical in mitigating its impact and protecting both human and animal health.
Avian Influenza Medication and Vaccines
Current Treatment Options
Overview of Antiviral Medications Available for Treating Bird Flu in Humans
When it comes to treating avian influenza (bird flu) in humans, antiviral medications are the primary line of defense. These medications, particularly neuraminidase inhibitors like oseltamivir (Tamiflu) and zanamivir (Relenza), are designed to inhibit the replication of the influenza virus within the body, thereby reducing the severity of symptoms and preventing complications.
- Oseltamivir (Tamiflu): Oseltamivir is the most commonly prescribed antiviral medication for treating bird flu. It is effective against various influenza strains, including H5N1. When administered within 48 hours of symptom onset, oseltamivir can significantly reduce the duration of the illness and the risk of severe complications such as pneumonia. However, its effectiveness is diminished if the treatment is delayed beyond this window.
- Zanamivir (Relenza): Zanamivir is another neuraminidase inhibitor used to treat bird flu. Unlike oseltamivir, which is taken orally, zanamivir is administered through inhalation. It is particularly useful for patients who are unable to tolerate oral medications. Similar to oseltamivir, zanamivir is most effective when given early in the course of the illness.
- Peramivir (Rapivab): Peramivir is an intravenous antiviral medication used in cases where oral or inhaled antivirals are not feasible, particularly in severe cases of bird flu. It is typically reserved for hospitalized patients who require immediate and aggressive treatment.
- Baloxavir Marboxil (Xofluza): This newer antiviral medication works by inhibiting the endonuclease enzyme, which is essential for viral replication. Although primarily used for seasonal influenza, baloxavir marboxil has shown potential in treating bird flu strains as well. However, its use is still under investigation for avian influenza.
Effectiveness of Current Treatments and Challenges in Treating Severe Cases
While antiviral medications can be effective in treating bird flu, their success is contingent on several factors:
- Timely Administration: The effectiveness of antiviral medications is highly dependent on how quickly they are administered after symptom onset. Delayed treatment reduces the likelihood of preventing severe complications and improving outcomes.
- Resistance: There have been instances where H5N1 and other avian influenza strains have developed resistance to antiviral medications, particularly oseltamivir. This resistance poses a significant challenge, as it limits the available treatment options and necessitates the development of new drugs.
- Severity of Infection: In severe cases of bird flu, particularly those involving respiratory distress and multi-organ failure, antiviral medications alone may not be sufficient. Such cases often require intensive care, including mechanical ventilation and supportive treatments to manage complications.
- Limited Availability: In some regions, access to antiviral medications may be limited, particularly in developing countries where healthcare resources are scarce. This can exacerbate the impact of bird flu outbreaks and increase mortality rates.
Vaccine Development

Progress in Developing a Vaccine Against H5N1 and Other Bird Flu Strains
The development of a vaccine against H5N1 and other avian influenza strains has been a priority for global health authorities, given the potential for these viruses to cause widespread illness and death.
- H5N1 Vaccines: Several vaccine candidates have been developed specifically for the H5N1 strain. These vaccines typically use an inactivated or live-attenuated form of the virus to stimulate an immune response. Clinical trials have shown that these vaccines can induce a strong immune response in humans, providing protection against H5N1.
- Universal Flu Vaccines: In addition to strain-specific vaccines, researchers are working on developing a universal influenza vaccine that would provide broad protection against multiple flu strains, including avian influenza. Such a vaccine would be a significant breakthrough, as it could potentially reduce the need for annual flu vaccinations and provide protection against pandemic strains.
- Adjuvants: To enhance the effectiveness of bird flu vaccines, researchers are exploring the use of adjuvants—substances that boost the immune response. Adjuvanted vaccines have shown promise in producing a stronger and longer-lasting immune response, particularly in vulnerable populations such as the elderly.
Challenges in Creating an Effective Vaccine Due to the Virus’s Rapid Mutation
The development of a bird flu vaccine is fraught with challenges, largely due to the nature of the virus itself:
- Viral Mutation: Avian influenza viruses, including H5N1, are known for their ability to mutate rapidly. This genetic variability makes it difficult to create a vaccine that provides long-lasting protection, as the virus can evolve to evade the immune response generated by the vaccine.
- Vaccine Efficacy: The efficacy of bird flu vaccines can vary depending on the specific strain of the virus and the population being vaccinated. For example, vaccines that are effective against one strain may not provide adequate protection against a mutated version of the same virus.
- Production and Distribution: The production of bird flu vaccines is a complex and time-consuming process. In the event of a pandemic, the ability to produce and distribute vaccines on a large scale is a significant challenge. Ensuring equitable access to vaccines, particularly in low-income countries, is also a critical issue.
Status of Vaccine Trials and Expected Availability
As of 2024, several bird flu vaccines are in various stages of development and testing:
- Clinical Trials: Multiple clinical trials are underway to test the safety and efficacy of H5N1 vaccines in humans. These trials involve different formulations, including inactivated, live-attenuated, and recombinant vaccines. Early results have been promising, with several candidates showing strong immune responses in trial participants.
- Emergency Use Authorizations: In some cases, vaccines have been granted emergency use authorization (EUA) during outbreaks to protect high-risk populations, such as poultry workers and healthcare personnel. These EUAs allow for the rapid deployment of vaccines while additional data is being collected.
- Global Stockpiles: To prepare for a potential bird flu pandemic, organizations like the World Health Organization (WHO) and the U.S. Centers for Disease Control and Prevention (CDC) have established global stockpiles of H5N1 vaccines. These stockpiles are intended to provide an initial supply of vaccines in the early stages of an outbreak while mass production ramps up.
- Future Availability: The timeline for the widespread availability of a bird flu vaccine will depend on the outcomes of ongoing trials and the global demand for the vaccine. If a pandemic were to occur, efforts would likely focus on producing and distributing the vaccine as quickly as possible, with priority given to high-risk groups.
In conclusion, while significant progress has been made in the development of medications and vaccines for avian influenza, challenges remain in ensuring their effectiveness and availability. The rapid mutation of the virus, coupled with logistical hurdles in vaccine production and distribution, underscores the need for continued research and preparedness to mitigate the impact of future bird flu outbreaks.
7 Experts Advice on ‘Triple E,’ Massachusetts Deadly Mosquito Virus
Preventive Measures and Public Awareness
Guidelines for the Public


Advice on Avoiding Infection
Preventing avian influenza (bird flu) infections requires a combination of personal vigilance, adherence to public health guidelines, and staying informed about ongoing risks. For the general public, the most effective measures include:
- Avoiding Contact with Birds: The primary source of bird flu transmission to humans is through direct contact with infected birds, whether they are wild birds or domestic poultry. People are advised to avoid handling birds, visiting poultry farms, or coming into close contact with areas where birds congregate, such as wetlands or bird markets.
- Consuming Only Pasteurized Products: To reduce the risk of infection from contaminated food products, it is essential to consume only pasteurized dairy products and properly cooked poultry. Pasteurization kills harmful bacteria and viruses, including avian influenza viruses. Consumers should avoid raw or undercooked eggs, meat, and unpasteurized milk, as these can harbor the virus.
- Cooking Poultry Thoroughly: When preparing poultry at home, it is crucial to cook it to an internal temperature of at least 165°F (74°C) to ensure that any potential virus is destroyed. This precaution also applies to eggs, which should be cooked until both the yolk and white are firm.
- Hygiene and Sanitation Practices: Maintaining good hygiene is vital in preventing the spread of bird flu. Regular handwashing with soap and water, especially after handling animals or raw poultry, is essential. Using hand sanitizers with at least 60% alcohol can also help reduce the risk of infection. Additionally, avoiding touching the face, particularly the eyes, nose, and mouth, can prevent the virus from entering the body.
Importance of Hygiene and Sanitation for High-Risk Workers
Individuals who work in high-risk environments, such as poultry farms, slaughterhouses, or veterinary services, are at greater risk of exposure to bird flu. For these workers, stringent hygiene and sanitation practices are crucial:
- Personal Protective Equipment (PPE): Workers should wear appropriate PPE, including gloves, masks, goggles, and protective clothing, to minimize direct contact with potentially infected animals or contaminated materials.
- Decontamination Protocols: After working in high-risk environments, workers should follow decontamination protocols, including removing and sanitizing protective clothing and showering before returning home. This practice helps prevent the virus from being carried into other environments.
- Monitoring for Symptoms: High-risk workers should be vigilant about monitoring their health for early symptoms of bird flu, such as fever, cough, or difficulty breathing. If symptoms appear, they should seek medical attention promptly and avoid contact with others to prevent potential transmission.
- Vaccination: Where available, vaccination against seasonal influenza can provide partial protection against bird flu and is recommended for high-risk workers. This measure can also help reduce the likelihood of co-infection with multiple flu strains, which could lead to viral reassortment and the emergence of new strains.
Government and International Initiatives
Overview of Government Efforts to Monitor and Control Bird Flu
Governments worldwide have implemented various measures to monitor, control, and prevent the spread of bird flu. These efforts include:
- Surveillance Programs: National and regional surveillance programs are in place to detect bird flu outbreaks in wild birds, poultry, and other animals. Regular monitoring of bird populations helps identify outbreaks early, enabling swift response measures to contain the virus and prevent it from spreading to humans.
- Culling and Quarantine Measures: In the event of an outbreak, governments may implement culling (the mass slaughter of infected or at-risk animals) to control the spread of the virus. Quarantine zones are established around affected areas to limit movement and reduce the risk of further transmission.
- Public Health Campaigns: Governments run public health campaigns to raise awareness about bird flu, providing information on how the virus spreads, symptoms to watch for, and preventive measures the public can take. These campaigns are crucial in ensuring that people remain informed and vigilant.
- Research and Development: Governments support research into bird flu vaccines, antiviral treatments, and diagnostic tools to enhance preparedness and response capabilities. Funding is also directed toward understanding the virus’s evolution and potential for human-to-human transmission.
Role of International Organizations
International organizations play a critical role in coordinating the global response to bird flu:
- World Health Organization (WHO): The WHO monitors global bird flu activity, provides guidance to member states on prevention and control measures, and facilitates the sharing of information and resources. The WHO also leads efforts to develop vaccines and antiviral medications for bird flu and maintains global stockpiles for emergency use.
- Centers for Disease Control and Prevention (CDC): The CDC conducts research on bird flu, develops diagnostic tests, and provides technical support to countries dealing with outbreaks. The CDC also works closely with other international agencies to track the virus’s spread and assess the risk to public health.
- Food and Agriculture Organization (FAO): The FAO collaborates with countries to improve biosecurity measures in agriculture, particularly in the poultry industry, to prevent the spread of bird flu. The FAO also assists in the implementation of culling, vaccination, and surveillance programs in affected regions.
- World Organisation for Animal Health (WOAH): The WOAH (formerly OIE) sets international standards for animal health, including guidelines for managing bird flu outbreaks in livestock and wildlife. The organization also works to improve global veterinary services and disease reporting systems.
Future Preparedness
Importance of Preparedness for a Potential Pandemic
The possibility of a bird flu pandemic, potentially more severe than COVID-19, underscores the need for robust preparedness measures. Key aspects of preparedness include:
- Pandemic Planning: Governments and health organizations must develop and regularly update pandemic preparedness plans, which outline strategies for surveillance, containment, treatment, and vaccination. These plans should consider various scenarios, including worst-case situations, and ensure that resources are allocated appropriately.
- Stockpiling of Medical Supplies: Maintaining stockpiles of antiviral medications, vaccines, personal protective equipment, and other critical medical supplies is essential to ensure a rapid response in the event of a bird flu pandemic. These stockpiles should be regularly reviewed and replenished as needed.
- Research and Innovation: Continued investment in research is vital to improve our understanding of avian influenza, develop more effective vaccines, and explore new antiviral treatments. Innovation in diagnostic technologies, such as rapid testing methods, can also enhance early detection and response efforts.
- Public Education and Communication: Effective communication with the public is crucial during a potential pandemic. Authorities must provide clear, accurate, and timely information to guide public behavior, reduce panic, and encourage adherence to preventive measures. Lessons learned from COVID-19 highlight the importance of combating misinformation and maintaining public trust.
Lessons Learned from COVID-19
The COVID-19 pandemic has provided valuable lessons that can be applied to future outbreaks of bird flu:
- Global Collaboration: The global response to COVID-19 demonstrated the importance of international collaboration in sharing data, resources, and expertise. Similar collaboration will be necessary to address a bird flu pandemic, with countries working together to monitor the virus, develop treatments, and distribute vaccines.
- Healthcare System Resilience: COVID-19 exposed vulnerabilities in healthcare systems, particularly in terms of capacity, staffing, and supply chains. Strengthening healthcare infrastructure, ensuring adequate staffing, and improving supply chain resilience are critical for managing future pandemics.
- Equitable Access to Vaccines and Treatments: The unequal distribution of COVID-19 vaccines highlighted the need for equitable access to vaccines and treatments during a pandemic. Efforts must be made to ensure that all countries, regardless of income level, have access to life-saving interventions.
- Behavioral Adaptation: Public willingness to adopt preventive behaviors, such as mask-wearing, social distancing, and vaccination, was key to controlling COVID-19. Similar behavioral adaptations will be necessary to prevent and control a bird flu pandemic, requiring clear public health messaging and community engagement.
In conclusion, the prevention and control of avian influenza require a comprehensive approach involving individual, governmental, and international efforts. By learning from past experiences and maintaining vigilance, the global community can better prepare for and mitigate the impact of future bird flu outbreaks.
Conclusion
Summary of Key Points
The threat of bird flu, particularly the H5N1 strain, poses a significant concern for both public health and global stability. As outlined, the virus’s ability to spread from birds to humans, its potential for mutation, and the severe symptoms it can cause highlight the importance of vigilance. The ongoing spread of avian influenza across multiple regions, including its recent detection in mammals and dairy cattle, underscores the virus’s evolving threat. Preventive measures, public awareness, and adherence to health guidelines remain critical in mitigating this risk.
Furthermore, the impact on agriculture and the economy, coupled with the potential for human-to-human transmission, necessitates a coordinated response. The global community must prioritize surveillance, research, and vaccine development to stay ahead of the virus. The lessons learned from the COVID-19 pandemic also serve as a stark reminder of the importance of preparedness, equitable access to resources, and robust healthcare systems.
Final Thoughts
Staying informed and proactive is crucial in the fight against bird flu. The public should adhere to recommended guidelines, such as avoiding contact with potentially infected birds, consuming only pasteurized products, and practicing good hygiene. For those in high-risk environments, extra precautions are essential to prevent infection.
Continued research is vital to understanding the virus’s behavior, developing effective treatments, and creating vaccines. Global cooperation, spearheaded by organizations like the WHO, CDC, and FAO, is essential to monitor the virus’s spread, share knowledge, and coordinate responses. As the world navigates this ongoing threat, the need for vigilance, preparedness, and collaboration cannot be overstated. By working together and staying informed, we can minimize the impact of bird flu and prevent it from becoming the next global pandemic.



